How Does Hyperbaric Oxygen Therapy Help Treat IBD?
Northwestern Medicine Physician Conducting Groundbreaking Research
Published April 2023
The Centers for Disease Control and Prevention (CDC) estimates that there are more than 3 million people in the U.S. living with inflammatory bowel disease (IBD), a broad term that indicates chronic inflammation of the gastrointestinal tract and includes Crohn’s disease and ulcerative colitis.
There is a lot of hope for patients with ulcerative colitis.— Parambir S. Dulai, MD
When someone has ulcerative colitis, the lining of their colon breaks down. Depending on the disease’s severity, it can cause bloody diarrhea and abdominal pain, or even an uncontrollable urge to use the restroom, which forces patients to be close to a bathroom or results in accidents. It can be debilitating and can dramatically reduce a person’s quality of life.
For 10 years, Parambir S. Dulai, MD, gastroenterologist at Northwestern Memorial Hospital, has dedicated his time to researching how hyperbaric oxygen therapy might be able to help patients hospitalized with ulcerative colitis. The hope is that this type of therapy could transform the way the disease is treated.
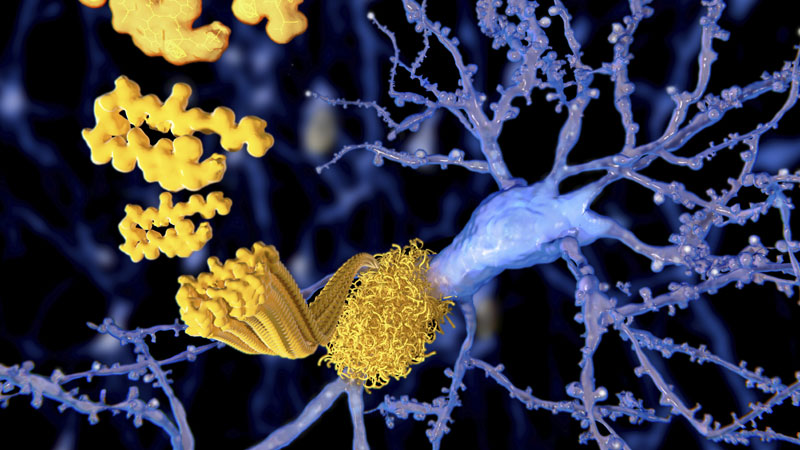
In response to ulcerative colitis, the body sends immune cells into the colon to try to help it heal. Immune cells consume all the oxygen as they try to fight off bad bacteria, but this eventually leads to a lack of oxygen in the tissue and makes healing more difficult. Hyperbaric oxygen therapy pushes oxygen into the colon through its tiny blood vessels. This kills the inflammation-causing bad bacteria that thrive in these low-oxygen environments. It resets the immune system and allows the colon to heal.
“The patients inspired me – how young they often were, and how many unanswered questions there are about these diseases,” says Dr. Dulai, “When I started this research, there was almost 100% disbelief that it would work. But this study is helping prove there is a lot of hope for patients with ulcerative colitis and a promising future of this method of treating the disease.”
The Science Behind It
During hyperbaric oxygen therapy, the patient is inside a hyperbaric oxygen therapy chamber with higher-than-normal air pressure. This allows the patient’s lungs to gather much more oxygen. The extra oxygen helps fight bacteria and promotes healing.
For Dr. Dulai’s study, patients were placed in the hyperbaric chambers for two hours a day for five consecutive days. While in the chamber, patients rested, listened to music or watched movies. They received pressurized 100% oxygen, and the results surpassed even the researchers’ expectations.
“It sounded too good to be true. But up to that point, nobody had really been successful at putting science behind the observations,” Dr. Dulai says. “However, within five days, their bleeding was gone. These patients were the sickest of the sick, and they were just days away from major surgeries to remove their colons. When you get to that point with ulcerative colitis, you’re no longer eligible for pharmaceutical trials, and few treatments have been studied for these patients.”
A Promising Future
In March 2023, the National Institute of Diabetes and Digestive and Kidney Disease awarded a $12 million-dollar grant to fund a phase 3 clinical trial that would be conducted at 20 sites across the country. This will enable more clinician-scientists to keep studying the use of hyperbaric oxygen therapy to treat patients who are hospitalized for ulcerative colitis flares. Dr. Dulai will partner with the Northwestern University Data Analysis and Coordinating Center, led by Lauren Balmert Bonner, PhD, and with colleagues at Northwestern Medicine Lake Forest Hospital, which is home to the health system’s in-hospital hyperbaric chambers.
“This study is especially exciting for patients who are in rural areas that do not have access to world-class physicians who specialize in inflammatory bowel disease,” Dr. Dulai said. “If we can get these patients out of the hospital and home to begin effective treatments, then they will be less likely to need life-changing surgeries. Access to care and financial resources should never be factors that determine why some people get to keep their colons while others don’t.”
The phase 3 clinical trial will study another element of hyperbaric oxygen therapy: its long-term effectiveness in treating ulcerative colitis.
“Three months after we treated patients in the first study, we realized they weren’t coming back to the hospital, and they were able to spend a couple of months healing and choosing new medication options,” Dr. Dulai said. “It appears that the treatment gave them several months to feel empowered to manage their disease and gave their physicians time to make an informed decision about the next treatment option. The next study will examine how patients are doing 12 months after their initial treatments. It will provide a framework so we can understand the durability of this approach in the outpatient setting. We will also learn more about whether we need to provide outpatient treatments to maintain the response to hyperbaric therapy.”
In five years, he’s hopeful that this trial will lead to the first FDA-approved treatment developed outside of the pharmaceutical industry.
“We have great medications for ulcerative colitis, but at the same time, 70% of people will lose response to them within a few years,” Dr. Dulai said. “At least half of the people who have ulcerative colitis will be hospitalized at some point in their disease. To realize a simple treatment like hyperbaric oxygen therapy could have life-changing benefits for these patients is very exciting. Many of the patients we treated are still sending us thanks for the care they received.”