Barely Breathing
Published February 2020
Father Emerges From a Coma
In the emergency department, Mike Barr was struggling to breathe. He hunched over and looked down at his boots. That was the last thing he remembered until he woke up — a month later — at a different hospital.
Meet Mike: A Personality to Be Reckoned With
Mike, 51, is a husband, a father of three, a pipefitter — and a man full of energy and personality. But over time, he started feeling fatigued and had difficulty breathing. “I was slowly deteriorating as far as breathing,” he says. “But I chalked it up to being out of shape, and I didn’t pay much attention to it.”
I was slowly deteriorating as far as breathing.— Mike Barr
At the end of a long day of physically demanding work, Mike decided it was time to seek medical attention when breathing became a struggle just to walk a couple feet. He arrived at Northwestern Medicine McHenry Hospital just as his breathing completely failed. “The next thing I remember is waking up in a hospital room and asking the nurse where I was,” he says. It was one month later, and he was at Northwestern Memorial Hospital.
During that month, Mike had been in an induced coma. After the first two weeks in a coma, he was transferred to Northwestern Memorial Hospital to get the specialized care required for his condition. He had acute hypoxic respiratory failure, a condition in which there is not enough oxygen in the blood. Subsequently, he was fighting an infection, requiring aggressive therapies over a month. His prognosis was not good. “They were planning my funeral while I was on the ventilator,” Mike reveals.
Thankfully, during that first month in a coma and the ensuing months in the hospital and recovery, Mike had a collaborative care team across both hospitals that never stopped fighting for him.
Getting to the Heart of the Matter
Mike’s physicians discovered that he had recurrent pulmonary embolisms: dangerous blood clots that had travelled through his legs, into his lungs, causing his breathing difficulties. This resulted in a form of high blood pressure in the lungs known as chronic thromboembolic pulmonary hypertension (CTEPH), causing failure of the right ventricle of his heart.
“Acute pulmonary embolism can be life-threatening, but luckily we have many therapies available. When clots are present chronically, this can be debilitating. There are few centers that can manage severe cases,” explains Northwestern Medicine Interventional Cardiologist Daniel R. Schimmel, MD. Dr. Schimmel says these cases require anticoagulation, a treatment that slows the blood’s ability to clot, which can keep existing clots from growing larger, help prevent future ones from forming and allow the body to dissolve the clot. But clots don’t dissolve for everyone, leading to scarring in the lungs.
“The reason people have these scarred tissues in the lungs is they’ve had previous blood clots that have become chronic,” says Northwestern Medicine Cardiothoracic Surgeon S. Christopher Malaisrie, MD. “These clots can then have the potential to completely obstruct blood flow to the lungs, causing you to become very symptomatic.”
Typically, three types of therapy — medical, surgical and catheter-based — will be considered to treat clots. Because Northwestern Medicine Bluhm Cardiovascular Institute offers a unique multidisciplinary program that brings a team of specialists together to guide patient care, Dr. Malaisrie and Dr. Schimmel collaborate to assess which combination of techniques will be most beneficial for each individual. “What makes this special is we regularly collaborate on interventional and surgical care to decide what’s best for you,” explains Dr. Malaisrie.
Together, they consider a number of factors on an individual basis, including the overall health of the patient. “The surgery is very long,” says Dr. Schimmel, who explains that the surgery can be risky if the patient has additional medical issues. “The second aspect we consider is the location of the clots and the overall clot burden.”
In Mike’s case, Dr. Malaisrie performed the first procedure: a pulmonary endarectomy. This is a technically difficult surgical procedure that removes the clots, or fibrotic scars, from inside the artery that goes to both of the lungs. After Dr. Malaisrie removed three larger clots, Dr. Schimmel proceeded to break up clots and restore blood flow with a procedure known as balloon pulmonary angioplasty (BPA). Under local anesthetic, Dr. Schimmel is able to thread a narrow tube through the femoral vein in the leg, up into the chambers of the heart and into the arteries in the lungs.
Time to Breathe Better
The road to recovery was “brutal,” admits Mike. “I don’t beat around the bush. When I coughed, it felt like somebody was driving over me with a car. But I’ll tell you this, it was so worth it.”
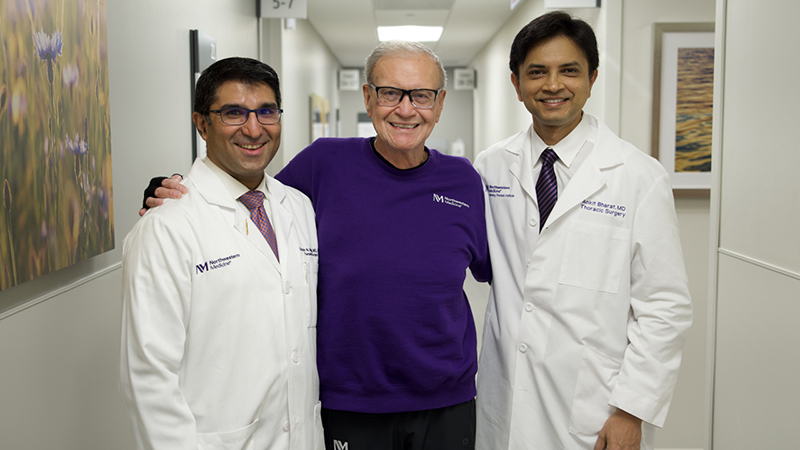
“He put a lot of faith in us, and that meant a lot,” says Dr. Schimmel. “He really was on his deathbed. But not only did we help him survive, we gave him back a great quality of life.”
“Mike could barely breathe at that time,” adds Dr. Malaisrie. “This procedure is incredibly satisfying because the difference before operation and after operation is apparent immediately.”
Mike agrees, saying, “I’m back to my normal self.” He was eager to resume working and provide for his family, and has since been able to go on a vacation to Colorado, a surprise for his birthday. “I was able to walk and spend time going up in the elevation, where the air is a lot thinner,” he says. “And I was breathing.”