Emergency Care for Expectant Mother Leads to Life-Saving Melanoma Tumor Discovery
From 36-Week Pregnancy to Emergency Cesarean Birth and Cancer Treatment
Published December 2024
While pregnant with her first child, MaKenna Lauterbach developed a cough that wouldn’t go away. The then 26-year-old, who lives on a farm with horses and goats in Washburn, Illinois, mentioned the cough to her local care team, but because she was pregnant, her clinicians were reluctant to perform chest scans due to possible radiation exposure.
MaKenna was in real trouble, and we had to act quickly.— Lynn M. Yee, MD
“I give hay to the horses every morning and noticed how winded I was becoming with a dry cough. My body felt like I just ran two miles, when in reality, I had only walked to the barn and back,” says MaKenna. “I knew something was wrong.”

By the time MaKenna was 36-weeks pregnant, the cough was so bad that she started throwing up while coughing. After she was hospitalized for shortness of breath, physicians obtained imaging and discovered a large, grapefruit-sized tumor in her middle chest cavity and right lung, completely blocking the artery to the right lung. MaKenna was in respiratory distress, which meant both she and the baby weren’t getting enough oxygen.
Due to her critical condition, MaKenna was flown to Northwestern Memorial Hospital in Chicago and rushed to an intensive care unit where a large team of obstetricians, surgeons, anesthesiologists, pediatricians and nurses were waiting for her. There, the maternal-fetal medicine team also noticed MaKenna’s blood pressure was rising, she was contracting and the baby wasn’t tolerating the contractions well.
“MaKenna was in real trouble, and we had to act quickly — this wasn’t something that could wait for Monday morning,” explains Lynn M. Yee, MD, a maternal-fetal medicine specialist at Northwestern Medicine. “When you’re pregnant with a baby that’s nearly full-term, your lungs already aren’t functioning at full capacity. When you add a huge tumor on top of it, you run the risk of having respiratory collapse and cardiac arrest.”
In the early hours of March 31, Dr. Yee performed an emergency cesarean section and a healthy baby boy named Colter was born. He remained in the neonatal intensive care unit (NICU) at Northwestern Medicine Prentice Women’s Hospital for one week, where the family formed a connection with the nursing staff, especially clinical nurse Mary Schuessler.
“Because of the tumor, the delivery happened so quickly. I was grieving the birth plan I had spent months preparing for, while also dealing with the news of my unexpected diagnosis,” says MaKenna. “My situation was serious, and while my clinical team was working on a plan to treat my cancer, it was comforting to know that Mary and the rest of the NICU nurses were taking such wonderful care of our son. My husband (Parker) and I can’t thank them enough.”
Making the Diagnosis and Developing a Treatment Plan
Following the delivery, doctors needed to figure out what type of tumor MaKenna had. Kalvin C H Lung, MD, a thoracic surgeon with the Northwestern Medicine Canning Thoracic Institute, was able to obtain a sample of the tumor with advanced bronchoscopy to diagnose MaKenna with stage 3 melanoma. Knowing the benefit of a team approach to provide the most innovative treatments, Dr. Lung reached out to Sunandana Chandra, MD, a medical oncologist with the Robert H. Lurie Comprehensive Cancer Center of Northwestern University at Northwestern Memorial Hospital, to see if there was anything to offer MaKenna to help shrink the tumor before surgery.
“MaKenna’s diagnosis was difficult to make because we weren’t sure if the melanoma started in the chest or somewhere else,” says Dr. Lung. “There isn’t much literature or published cases on how to best treat tumors like these, so we had to rely on the expertise that we’ve developed here at Northwestern Medicine.”
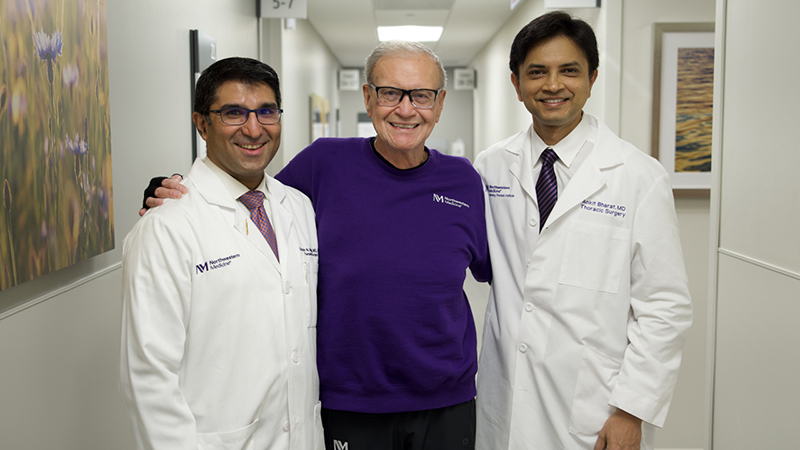
Based on a nationwide clinical trial that Northwestern Medicine was involved in, researchers discovered that pre-surgical immunotherapy can improve surgical outcomes for advanced melanoma patients. Dr. Chandra recommended MaKenna go through three cycles of immunotherapy before surgery, which helped shrink the tumor from 13 centimeters to 9 centimeters, allowing Dr. Lung and Christopher K. Mehta, MD, a cardiac surgeon with the Northwestern Medicine Bluhm Cardiovascular Institute who specializes in complex heart reconstruction, to remove MaKenna’s entire right lung, parts of the main pulmonary artery and lymph nodes.
“The tumor was sitting on top of MaKenna’s heart and extended into the right lung, impacting all three lobes and the entire main trunk of the pulmonary artery, which is why we had to remove the right lung,” says Dr. Lung.
“It's extremely rare to see this type of tumor invading into the major blood vessels of the heart,” adds Dr. Mehta. “We may see something like this once every few years.”
“We think at some point, MaKenna had a melanoma on her skin and her own immune system took care of it, but not before a cell or two may have escaped and eventually started growing inside her body,” explains Dr. Chandra. “MaKenna’s scans currently show no evidence of metastatic melanoma, and the hope is with continued surveillance, we’ll continue to show she has no evidence of disease. Medically, this is an amazing story with profound results. This type of outcome for our patients is what we always hope for.”
Looking Forward to the Future as a Family
MaKenna will continue immunotherapy treatments for one year. She celebrated her 27th birthday in October and is looking forward to her son’s first Christmas on the farm.
“Colter's the best baby. He's always happy and sleeps through the night,” says MaKenna. “I’m so grateful to have Colter and Parker in my life, and I can’t say enough about the wonderful medical team that saved my life. Because of Northwestern Medicine, I’m here today.”

“It brings tears to my eyes to see MaKenna doing so well, and seeing Colter thriving is amazing,” says Dr. Yee. “It just goes to show that when you get all the right medical teams in place, you can truly help families thrive.”
Learn about the stages of cancer and how a stage represents more than just the extent of the disease.