Surgeons Use an Artificial Lung and Breast Implants to Save a Man Who Needed a Double-Lung Transplant
Innovative Procedure for 34-Year-Old Whose Lungs Were Infected With Influenza
Published November 2023
Before 34-year-old David “Davey” Bauer was in the Intensive Care Unit (ICU) at Northwestern Memorial Hospital living without lungs, he enjoyed snowboarding, skateboarding, gaming and golfing. He worked in landscaping and hardscaping in De Soto, Missouri. Davey started smoking cigarettes when he was 21 years old and switched to vaping in 2014.
“Vaping felt better, and I thought it was the healthier alternative,” he says, “But in all honesty, I found it more addicting than cigarettes.”
Davey’s lungs were so heavily infected that they started to liquify.— Rade Tomic, MD
In April 2023, Davey started experiencing shortness of breath and was diagnosed with influenza A (the flu), which he hadn’t received a vaccination for. He developed a lung infection that was resistant to antibiotics. Up until that point, he had never been seriously ill. He was admitted to a hospital in St. Louis and placed on extracorporeal membrane oxygenation (ECMO), a device that does the work of the heart and the lungs. Davey continued to decline, and a double-lung transplant became his only option for survival. However, due to the severity of his infection, this option came with several challenges.
An Artificial Lung and DD Breast Implants
“Davey’s lungs were so heavily infected that they started to liquify. If you looked at his X-ray, there was nothing left — the lungs were completely filled with pus,” says Rade Tomic, MD, pulmonologist and medical director of the Northwestern Medicine Lung Transplant Program at Canning Thoracic Institute. “When we received a call from Davey’s medical team in St. Louis, we thought we could help him, but it was also very clear he wouldn’t survive the transplant in his current condition. He needed to clear the infection before we could list him for transplant, but the only way to do that was to remove both lungs. This was unchartered territory for us, but our team knew if we couldn’t help Davey, no one else could.”
The surgical team at Northwestern Medicine Canning Thoracic Institute quickly came up with a strategy to remove the infected lungs and engineer a novel artificial lung that could attach to Davey’s body to keep blood flowing to his heart, brain and organs. This artificial lung was different from ECMO. To be on ECMO, patients need to have both lungs in their chest cavity. The device the Canning Thoracic Institute team created did the work of the lungs without the lungs. With both lungs removed, surgeons needed a way to keep Davey’s heart from physically collapsing inside his chest cavity, and that’s where the idea for DD breast implants came in.

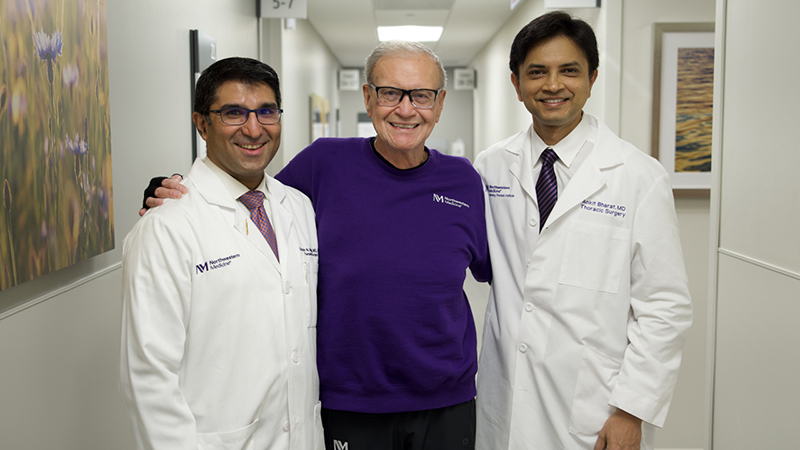
“One of our plastic surgeons was very gracious to give us a rapid-fire course on the different types, shapes and sizes of breast implants, so we picked out a couple options and some of them were easier than others to mold inside Davey’s chest, with the DD option being the best fit,” explains Ankit Bharat, MD, chief of Thoracic Surgery and director of Canning Thoracic Institute. “I never imagined we’d be using DD breast implants to help bridge a patient to lung transplantation, but our team is known for taking on difficult cases and thinking outside the box to save lives.”
Once the infected lungs were removed on May 26, 2023, Davey’s body immediately started clearing the infection and he was listed for a double-lung transplant. The team received an offer for new lungs the next day, and on May 28, 2023, Davey’s surgical team removed the breast implants and put in the donor lungs. Davey spent several months recovering in the ICU at Northwestern Memorial Hospital before being discharged to rehabilitation therapy in late September 2023.
“Davey’s case is remarkable because it shows that we can keep patients alive after removing their lungs through new technology, which can be transformative for many critically ill patients,” says Dr. Bharat. “With this new approach that we’ve developed, many patients who get to the point of needing a lung transplant — but their damaged lungs are making them too sick to get one — can now potentially get transplanted. I think it’s going to open a lot of doors for many patients who have no other options.”
“DD Davey”
Because they helped save his life and he was the first Northwestern Medicine patient to have both lungs removed and breast implants temporarily put in their place, Bauer jokes that his new nickname is “DD Davey.”
“Still to this day, I can’t believe Davey lived without any lungs. He was breathing, blood pumping without lungs,” says Davey’s girlfriend and caretaker Susan Gore. “While we waited inside his hospital room at Northwestern Memorial Hospital, I would take a breath in and say, ‘one breath for me and one for Davey.’ It’s hard to wrap my mind around it, and I’m still in awe that Davey was able to do this — it truly shows his strength.”
As of November 2023, Davey remains in Chicago so his transplant team can continue to closely monitor him. While he misses St. Louis, he’s looking forward to enjoying the holidays in a new city with his new lungs.
“I’m so grateful to be alive and know I wouldn’t be here today without the support of my girlfriend, family, friends and my Northwestern Medicine transplant team who never gave up on me,” says Bauer. “If I could go back in time, I never would have picked up a cigarette or vape pen, and I hope my story can help encourage others to quit, because I wouldn’t wish this difficult journey on anyone.”
If you are interested in being evaluated for a lung transplant at Northwestern Medicine, you can call the referral line at 844.639.5864.