Better Breathing for Severe COPD
Published October 2019
Tiny Valve, Huge Impact
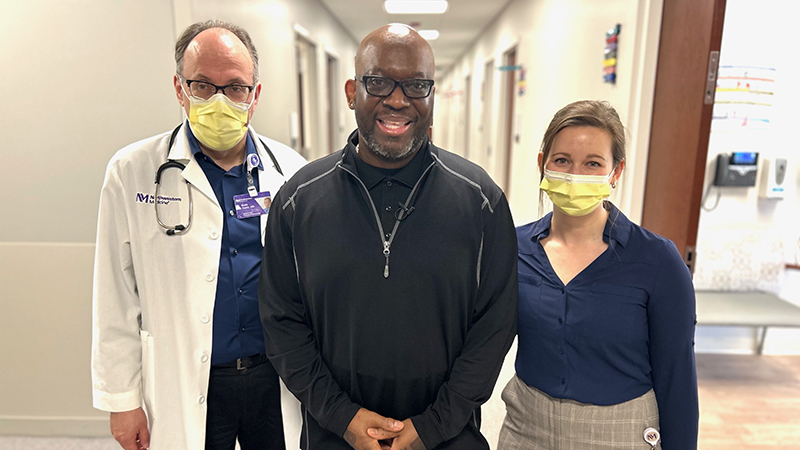
Once a businessman with a busy social calendar, Cy Kennedy of Wheaton found himself stuck at home due to emphysema, a severe form of chronic obstructive pulmonary disease (COPD). Now, after undergoing a minimally invasive procedure at Northwestern Medicine Central DuPage Hospital, Cy is looking forward to getting out of the house and back to the activities he enjoys.
New Procedure Provides Relief for Emphysema
According to the American Lung Association, more than 15 million people in the U.S. have COPD, and 4.7 million of those patients have emphysema. Emphysema destroys the elastic fibers in the lungs that hold open the small airways that lead to the air sacs. This causes the airways to collapse on exhale, preventing air in the lungs from escaping.
There are few treatment options for most patients with emphysema, and there is no cure. But one leading-edge procedure is bringing relief for patients like Cy. The Zephyr ® Endobronchial Valve System is the first FDA-approved, minimally invasive procedure to help those with emphysema breathe easier without major surgery. The procedure is done during a bronchoscopy using a thin tube containing a light, camera and small tools inserted into the lungs through the nose or mouth.
Tiny valves are placed in the airways to block off the diseased parts of the lungs. The valves reduce hyperinflation, or over inflation, preventing air from being trapped in the diseased area of the lung. This allows healthier parts of the lung to take in more air, resulting in easier breathing.
“Until now, the only other options for these patients were highly invasive treatments such as lung volume reduction surgery or lung transplantation,” says Benjamin J. Seides, MD, director of Interventional Pulmonology at Northwestern Medicine Central DuPage Hospital. “These small valves have the potential to be a life-changer for patients who struggle with each breath.”
The procedure is also offered at Northwestern Memorial Hospital.
Living With COPD
A week after undergoing the procedure, Cy says he took his best and deepest breath in 10 years and walked the farthest, without stopping and without a rescue inhalation, in three years.
“I’ve been a couch potato for over two years and had to turn down so many social events because I didn’t have the energy to leave my house,” says Cy. “My mind is young, and I want to get my body back.”
Dr. Seides is not surprised at Cy’s tremendous results. “Patients who previously consistently felt short of breath can enjoy a significantly improved quality of life,” says Dr. Seides. “It is extremely gratifying to see patients who were previously oxygen-dependent walk out of the hospital without supplemental oxygen.”
Today Cy is looking forward to getting back on the golf course, traveling and volunteering at a local nursing home. “When you lose your social life, it isn’t good,” he says. “I needed to do something, and I was thrilled I didn’t have to undergo surgery.”