Why Family Health History Matters
Published October 2019
The Story of Your Genes
You check in for your yearly exam. The receptionist hands you a clipboard and a pen. You swiftly fill out your name and contact information, but your pen stops at “Family History.”
Did your dad have high blood pressure? You can’t recall. Does it matter? He smoked, and you don’t. Though you may overlook this section and downplay it to your physician, your family’s health history matters.
“Family history is important because so many diseases have a genetic component,” says Northwestern Medicine Internal Medicine Physician and Pediatrician Rakhee Kalelkar, MD. “If we know about diseases that run in the family now, then we can start screening for them early — and often prevent them.”
Screening Your Genes
The importance of family history starts with your genes: pieces of DNA that your biological parents pass down to you that determine your traits, from the color of your eyes to the curls in your hair. They also determine your risk for certain medical conditions and disorders.
While you can’t change your genetic makeup, here’s why you should know your family medical history:
- You can change your lifestyle to reduce your risk of developing diseases that run in the family.
- You can start early screening for the diseases in your family tree.
- Family history gives your provider context.
- If you do develop a hereditary disease, it’s helpful to know what treatment options worked best for your family members. Chances are, they’ll also be effective for you.
- You can prepare for the care you may need to give a child.
“A lot of hereditary diseases, like high blood pressure and high cholesterol, can be staved off by maintaining a healthy diet and weight,” says Dr. Kalelkar.
Risk is unique for each disease and varies from time to time based on age, lifestyle choices and changes in medical history. Your physician can help personalize a prevention program that is based off your individual risk assessment.
“This applies especially to cancer history,” says Dr. Kalelkar. “For example, if you have a strong family history of breast or colon cancer, I’ll recommend starting routine screening earlier than the standard American Cancer Society suggestion of 40 and 50, respectively.”
Your physician may also recommend an increased frequency of screenings, such as mammograms or colonoscopies.
Some hereditary diseases don’t cause symptoms immediately. If your physician knows about your family history, they may recommend genetic testing for these diseases as a preventive measure.
By knowing your family history, your physician can connect any symptoms you may have to a disease that may run in your family. For example, if you see your physician with joint pain, they may consider rheumatoid arthritis in lieu of an overuse injury if they know you have a family history of autoimmune disorders.
“For people with a family history of mental illness like anxiety and depression, family history can inform treatment with medication,” says Dr. Kalelkar. “It’s helpful to know if a family member had a good reaction or result with one medication versus another.”
Similarly, if multiple members in your immediate family have had a blood clot, you may have a genetic predisposition to developing clots. As a result, your physician may take greater care or use caution when using medications like oral contraceptive pills, which can increase a woman’s risk of developing blood clots.
“Though women are screened for certain diseases during standard prenatal care, it’s important to know of any potential diseases that may run in the family or that other siblings may have had,” adds Dr. Kalelkar. “For example, we want to know if any siblings had jaundice or needed phototherapy for jaundice after birth. This may seem insignificant, but it helps your physicians assess risk and come up with a care plan for your newborn.”
During adolescence, your pediatrician may advise checking a lipid panel for a child with family history of early onset heart disease.
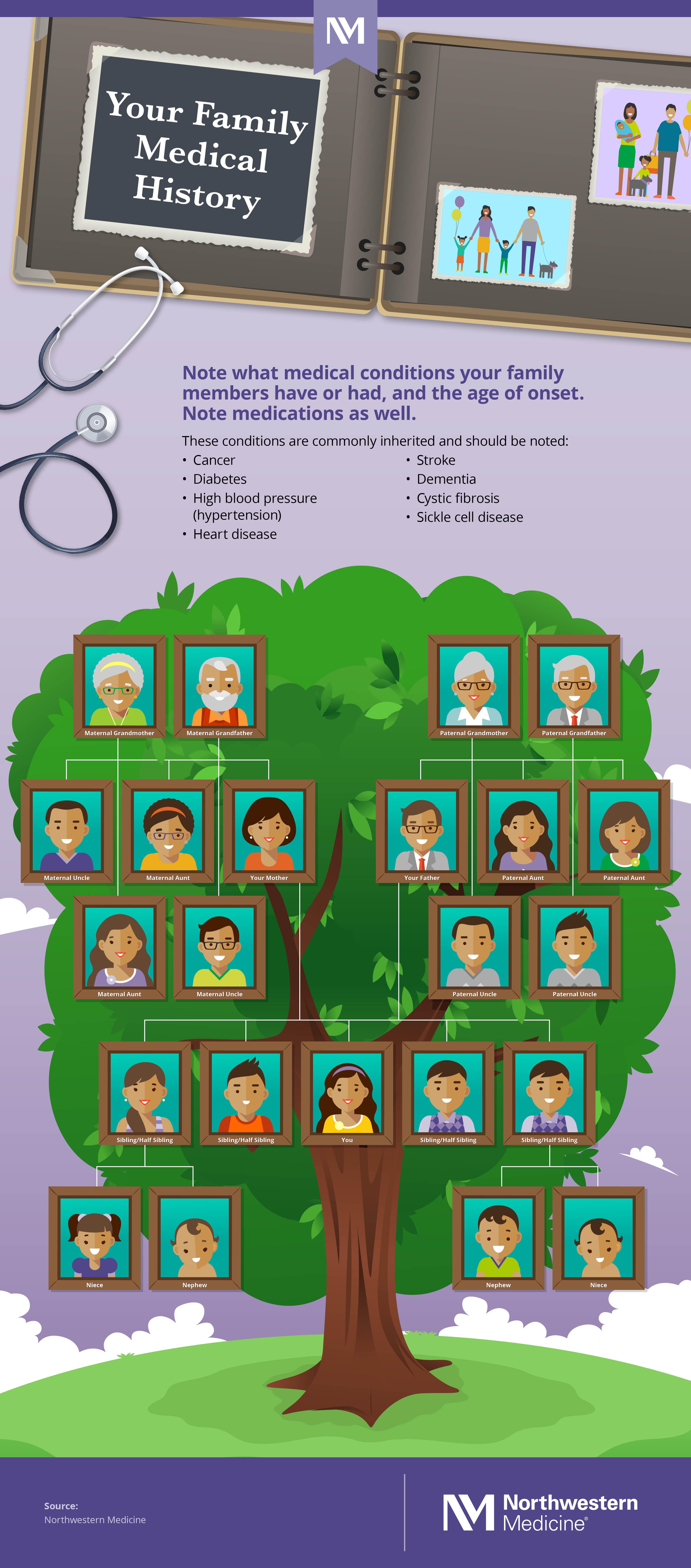
What should your family history include?
If possible, your family history should include family members’ names, their relationships to you and their current ages (or age of death). In addition to which conditions they may have or have had, the record should also include the age of onset. Provide history for first-degree (parent, sibling or children) and second-degree (grandparents, aunts, uncles, half-siblings, nephews and nieces) relatives.
Before you come to your next appointment, consult your family members and complete your family history tree to share with your primary care physician. Download and print the below graphic as a conversation starter.